Hi and welcome to my latest blog post about Nutrition for prconception & pregnancy. A couple of notes before you dive in. Firstly, a trigger warning; we do have a small discussion about miscarriage in this one. And secondly, I’m providing some general information here for you, however, I always recommend having a consult to ensure you’re receiving individualised preconception/pregnancy nutrition education that’s based on your needs.
Education based on your requirements is always going to be superior to general advice. I haven’t been able to go into great detail on some topics and there‘s so much information I wish I could include, but the purpose of this blog is to share with you some of the essentials and priorities in preconception/pregnancy nutrition.
Let’s begin!
It’s important to consider preconception and pregnancy nutrition as early as possible as good nutrition is the key to a healthy mum during her pregnancy and a healthy baby. Nutrition support can aid in reducing the risk of many pregnancy related health outcomes such as having a miscarriage and GDM (gestational diabetes mellitus). It’s been found that poor nutritional status has been implicated in miscarriage, particularly in relation to vitamin D, vitamin B6, B12 and folic acid deficiency. Nutrition can play a huge role in GDM, where the blood glucose levels increase due to a temporary reduction in insulin production by the pancreas. Eating a balanced diet and ensuring micronutrients such as zinc and iron are within the healthy reference range, before and during pregnancy, has been linked to lower implications of GDM in the third trimester.
The essentials
These are a few essential nutrients that should be supplemented in preconception and pregnancy. There may be others that are more applicable to your needs, so I stress the importance of having your blood tests done before you start your preconception journey to ensure you are supplementing accordingly. During an initial nutrition assessment and you’re subsequent follow up appointments, these are the primary biomarkers that are analysed from your blood tests. Appropriate supplementation options will be offered along with additional information and resources.
Folate (or folic acid) is needed for your baby to grow and develop. A large body of evidence supports the use of folic acid to lower the risk of neural tube defects (NTD) such as spina bifida.
It’s important to ensure you’re having adequate intake of folate in the months leading up to you falling pregnant and the first trimester (three months) of pregnancy. All women planning a pregnancy and in the early stages of pregnancy should take a folic acid supplement of at least 400-600mcg (micrograms) per day. You also get folate from eating a variety of folate-containing foods including green leafy vegetables such as broccoli, spinach, bok choy, and salad greens, some fruits, and cereals and breads with added folic acid.
Iodine
Adequate iodine in pregnancy is needed for your baby’s growth and brain development. Your body needs more iodine during pregnancy. All women who are pregnant, breastfeeding or considering pregnancy, should take a supplement of 150mcg (micrograms) of iodine. You still need to consume foods that are high in iodine. These include freshly cooked and consumed seafood, bread with added iodine, eggs and dairy.
Iron
Iron is important for foetal neurodevelopment, with iron deficiency during pregnancy shown to impair mental and psychomotor development. Iron is needed to form red blood cells for you and your baby. It helps carry oxygen in your blood and is needed for your baby to grow. During pregnancy you need a lot more iron than when you are not pregnant.
It is best to get the iron you need from your diet. The best sources of iron are lean meats (especially red meat), some vegetables (especially green leafy ones), legumes, and cereals with added iron. Iron from animal food sources is absorbed more easily than iron from plant foods.
You can help your body absorb iron from the food you eat or drink by:
- Including vitamin C with meals (e.g. citrus foods, tomato, capsicum)
- Including animal protein with green leafy vegetables at a meal.
- Using antacids sparingly
Some foods and drinks may stop your body using iron from your diet. To reduce this, avoid:
- Drinking tea or coffee with meals
- Taking your iron supplement with a meal that includes dairy
- Eating more than 2 tablespoons of unprocessed bran.
Omega 3 and eating fish
Fish is a safe and an important part of healthy eating. It is an excellent source of protein, is low in saturated fat, high in omega 3 fish oils and a good source of iodine. Omega 3 oils are important for growth of your baby’s brain and eye development.
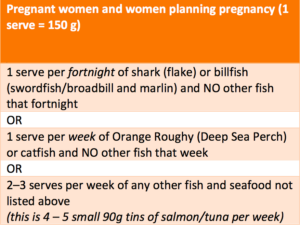
It is important to eat fish when you are pregnant but you need to be careful about the fish you choose. Some fish may accumulate mercury, which may be harmful to your baby’s developing nervous system. Food Standards Australia New Zealand has set the following safe guidelines for fish intake.
Nutrients and what they do
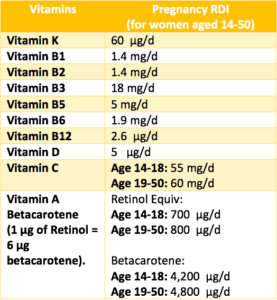
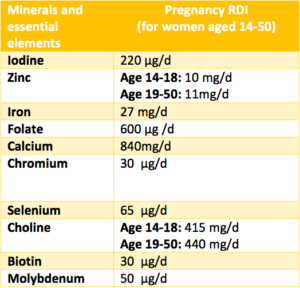
The below nutrient recommendations are the Australian standards, however, doses may vary between individuals. I like to stress that, although nutrients are important, it’ important to remember to eat food first and consider the individual nutrients after, unless it’s one of the essentials. If you’re deficient in a nutrient, it’s important to supplement as you need and if you’re having something in excess it’s important to find mindful ways to reduce your intake.
- Iron supports maternal energy and foetal brain development.
- Choline, lutein and omega-3 essential fatty acids support foetal brain development and enhance cognition and memory.
- Omega-3 fatty acids support foetal eye structure and function.
- Iodine is essential for foetal growth and development.
- Vitamin D, K2 and manganese support bone development.
- Vitamin B6 and ginger can reduce nausea and vomiting in pregnancy.
- Choline, omega-3, lutein, iron, zinc and vitamin B12 support child brain development.
Food First
It’s important to focus on nutrient rich meals, rather than meals that might restrict nutrients like discretionary foods that are high in saturated fats and refined sugar. Nutrient rich meals include a variety of vegetables, lean protein, wholegrain and cereals, dairy foods and fruits.
The table shows the recommended serves of each food group and a detailed list of what a serve of these foods would look like. These serving sizes and recommendations aim to meet all pregnancy and lactating nutrient requirements.
As an example, 1 serve of ‘grain/cereal foods’ is = ½ cup of cooked rice. When we eat cooked rice with a meal like a curry, you would more likely have 1 cup which means you’ve had 2 serves of grain foods. One cup of cooked rice gives you 4.2g protein, 44.5g carbohydrates, 0.4g fats as well as some micronutrients like folate, omega-3 fatty acids and selenium among others. You can see how each food eaten throughout the day will add up to meet the required nutrients.
During preconception and pregnancy, you shouldn’t heavily restrict foods or try to eat “perfectly”. There isn’t a perfect pregnancy diet, everyone will eat differently and require more or less of somethings, but the first step is to ensure you’re able to have a well-balanced diet to support your own health as well as bubs development and both of your future health.
Individualised support and recommendations may be required if you have a pre-existing medical condition that impacts your food intake, like coeliac disease, PCOS, lactose intolerance, IBS, diabetes, just to name a few.
| Food Group | Number of Serves per day (19-50 years) | 1 serve equals… |
| Vegetables and legumes/ beans | 5 | 1⁄2 cup cooked non starchy vegetables (e.g. broccoli, carrot, pumpkin or spinach)
1 cup raw salad vegetables |
| Fruit | 2 | 1 medium sized fruit (e.g. apple, banana, orange, pear) 2 pieces small fruit (e.g. apricot, kiwi fruit, plums)
30 g dried fruit (e.g. 11⁄2 tablespoons sultanas, 4 dried apricot halves) |
| Grain (cereal) foods, mostly wholegrain, | 8+1⁄2 (pregnancy term 2-3 + breastfeeding) |
1 slice of bread 1⁄2 medium bread roll or flat bread 1⁄2 cup cooked rice, pasta, noodles, polenta, quinoa, barley, porridge, buckwheat, semolina, cornmeal 2⁄3 cup breakfast cereal flakes 1⁄4 cup rolled oats or muesli 3 (35g) crispbreads 1 crumpet or 1 small English muffin or scone |
| Lean meat and poultry, fish, eggs, nuts and seeds, and legumes/beans | 3+1⁄2 | 65 g cooked lean red meats (e.g. beef, lamb, pork, venison or kangaroo) or 1⁄2 cup lean mince, 2 small chops, 2 slices roast meat
100 g cooked fish fillet or 1 small can fish, no added salt, not in brine 170 g tofu |
| Milk, yogurt, cheese and/or alternatives (mostly reduced fat) | 2+1⁄2 | 1 cup (250 ml) milk 40 g (2 slices) hard cheese (e.g. cheddar) 120 g ricotta cheese 200 g yoghurt |
| Additional serves for taller or more active women | 0–2+1⁄2 |
Additional serves from the five food groups or 2-3 dry/plain biscuits |
Other nutrients for consideration.
Fibre: 28g/day. Fibre comes from carbohydrate containing foods like wholegrain breads, cereals, rice, physillium husk, flax seeds, and many fruits and vegetables. Eating a wide variety of fruits, vegetables and wholegrains will ensure adequate fibre intake which helps to keep your bowel movements regular and your digestive tract free from obstructions that causes discomfort in the abdomen.
Sodium: 2300mg/d. Salt! It’s in and on everything and although we do need it, we don’t usually need to add it to our foods. High salt intake has been linked to high blood pressure, so this is a good one to slow down on during pregnancy. Look at the processed foods you’re eating and check the label for the sodium content and see if it is either Low (<
Water: 2800ml – 3100ml/d. it’s imperative to keep up your hydration. Not only do your requirements increase due to foetal growth, you’re likely to be excreting it much faster by the time you’re in the 2&3rd trimester and breastfeeding.
Alcohol & Caffeine: No amount of alcohol is safe to consume during pregnancy. It’s important to consider this when you’re entering your preconception journey. Slowly cutting down and finding ways to minimise it early on will make it easier for when you fall pregnant.
Caffeine is recommended to be minimised, however, there is a safe limit of about 200-300mg. This is 2-3 instant coffee’s or 1-2 espresso coffee. Remember to take into consideration any tea, energy drinks, soft drinks, and even milk chocolate. This also contributes to caffeine intake.
Managing food related side effects
Morning sickness; Many women suffer from sickness, usually in early pregnancy. Morning sickness is usually caused by changes in hormones, and can affect you at any time of the day. By the end of the 4th month of pregnancy, symptoms usually disappear or become much milder.
Some tips that may help morning sickness:
- Eat small amounts every two hours – an empty stomach can cause nausea.
- Avoid smells and foods that make your sickness worse.
- Eat healthier carbohydrate foods: try dry toasts or crackers, breakfast cereals and fruit
- Eat fewer fatty and sugary foods.
Heartburn; Heartburn, or reflux, is a burning feeling in the middle of the chest that can also affect the back of the throat. It is caused when acid moves from the stomach, back up the oesophagus. This happens because hormonal changes during pregnancy relax stomach muscles, and also because as the baby grows, more pressure is put on your stomach. Some tips to reduce heartburn:
- Eat small regular meals more often
- Avoid fatty, fried or spicy foods
- Avoid tea, coffee, carbonated drinks, chocolate drinks and alcohol
- Sit up straight while eating
- Do not bend or lie down after meals or wear tight clothes
- Sleep propped up on a couple of pillows.
- Eat in a calm, relaxed place
- Avoid peppermint and spearmint containing gums and herbal teas
- Avoid drinking at the same time as eating
Constipation; Constipation is common during pregnancy. Bowel motions can be slowed down by hormonal changes (relax the muscles in your bowel) and pressure from the growing baby. It is important to have enough fibre, fluid and physical activity to avoid constipation. Good sources of fibre include vegetables, fruit, wholegrain and high fibre breakfast cereals, wholegrain bread, nuts, seeds and legumes. Drink plenty of water.
Food Safety
Change to hormones during pregnancy may weaken your immune system. This can make it harder to fight infections. Foods can be a source of infections so protecting yourself from food poisoning is important.
Listeria
Listeria is a bacteria found in some foods, which can cause an infection called listeriosis. If passed on to your unborn baby, it can cause premature birth or miscarriage. It is important to avoid foods that are a high risk of containing listeria during pregnancy. These include:
- Unpasteurised dairy products
- Soft cheeses such as brie, camembert, ricotta, and fresh fetta, unless they are cooked (yellow, hard cheese, and processed packaged cheese are safe)
- Soft serve ice cream and thick shakes
- All paté and ready to eat cold meats, including deli and packaged meats (e.g. ham, salami, cooked chicken)
- Ready-to-eat salads (from salad bars, buffets, supermarkets)
- Raw or smoked seafood (including oysters, salmon, sashimi, sushi)
Some other bacteria can be harmful to your unborn baby. In addition to the precautions above: Do not eat raw or undercooked eggs. Eggs must be well cooked so that both the white and yolk are hard.
Always keep your food ‘safe’
- Choose freshly cooked and freshly prepared food.
- Avoid ready-to-eat food from salad bars, sandwich bars, delicatessens and smorgasbords.
- Thaw food in the fridge or defrost in the microwave.
- Cool left-over food in the fridge rather than the bench.
- Wash your hands, chopping boards and knives after handling raw foods.
- Make sure hot foods are hot (above 60 degrees Celsius) and cold foods are cold (below 5 degrees Celsius), both at home and when eating out.
- Make sure all food is fresh and used within the use-by date.
- Wash fruits and vegetables thoroughly
- Cook all meat, chicken, fish, and eggs thoroughly
- Reheat leftover foods to steaming hot (above 74 degrees) for over 2 minutes before eating.
- Eat leftovers within 24 hours or freeze
Questions?
If you have questions about your preconception/pregnancy nutrition needs, please get in touch and book for your initial consult.
Initial consults include; Analysis of nutritional status (nutrient deficiencies and pre-existing medical conditions), understanding your current food and nutrition knowledge, discussing your nutrition education needs, goal setting for implementing pregnancy nutrition, take home education resources for pregnancy nutrition. 2-3 follow up consults are required for ongoing care during pregnancy.
Follow up consults include; analysis of progress (improving nutritional status or implementing changes), understanding ongoing nutrition knowledge gaps and areas requiring further development, appropriate resources for ongoing care.
Thanks for reading
Jen Darnell | Nutritionist
Resources:
https://www.health.qld.gov.au/__data/assets/pdf_file/0028/154792/antenatal-heatwtgain.pdf
https://www.health.qld.gov.au/nutrition/patients
https://www.metagenicsinstitute.com.au/tech-data/key-nutrients-preconception-pregnancy
https://www.nrv.gov.au/nutrients-energy-calc#nutrition-results
